Financial Management: Level 1
Provide billing and coding education and tools to staff
Identify relevant codes for patient immunizations and provide appropriate staff members with ongoing education on and tools for proper usage and processes. Evaluate coding for accuracy and to inform future training opportunities.
Training providers and staff on how to properly code immunization services is critical to maintaining timely reimbursements and keeping your organization’s cash flow on track. To provide valuable billing and coding education and tools to staff, follow the steps below.
Step 1:
Identify relevant codes for immunization services
There are a variety of codes that providers and staff need to use for organizations to receive reimbursement for immunization services, including procedure codes (CPT, HCPCS), modifiers to procedure codes when more description is needed, and diagnostic codes (ICD-10).
When identifying relevant codes, remember:
- Many of these codes are updated on an annual basis, so appoint a team member—such as your organization’s Immunization Champion —to stay abreast of changes.
- Ensure there is a process in place for relevant code changes to be integrated into your organization’s electronic health record (EHR) and billing system, as needed, so they are available for use.
- Consult coding guidelines and your organization’s payers to understand bundling rules and compliant coding practices.
Step 2:
Educate providers and staff responsible for billing and coding
Determine the individuals responsible for billing and coding within your organization. Develop training and ongoing education to ensure those team members understand how and when to use required codes for immunization services. Education can take various forms and the timing/frequency will depend, in part, on which team members require training. Opportunities may include:
- Coding training during the orientation period for new employees in relevant jobs (e.g., coders and medical assistants involved in the entry process)
- Integrating coding training and updates for existing personnel during other scheduled training activities to optimize the time of busy providers and staff
- Appointing a specific staff member, such as your Immunization Champion, as a dedicated resource for immunization coding questions
- Keeping staff informed by making immunization codes and coding updates available via tools that are easy to access and modify (e.g., a dedicated page in an employee intranet instead of printed handouts)
Ensure education and training opportunities address the nuances associated with billing and coding for each vaccine, such as:
Influenza vaccines administered in outpatient settings may not have a reimbursable administration fee when an Evaluation and Management (E/M) code is billed at the same visit, absent a modifier 25 code being appended to the E/M code. Consult bundling rules, modifier guidelines, and payer policies to bill compliantly.
Pneumococcal vaccines for Medicare patients require that the ACIP-recommended intervals are observed between doses for reimbursement as well as for maximum immune response.
Tdap vaccines during pregnancy are not fully covered by all state Medicaid plans, with some plans only covering diphtheria and pertussis for the baby and not the tetanus component.
Zoster vaccines cannot be billed through either Medicare Part A or B, but can be billed through Part C, Part D, some commercial insurance plans, or when administered at a pharmacy. Most private payers are required to cover zoster vaccines for patients 50-64 years of age as recommended by the Advisory Committee on Immunization Practices (ACIP).
Step 3:
Update training and tools to address gaps in knowledge
Routinely revise your education and training materials to address any gaps in knowledge. Many organizations have a protocol in place for reviewing codes for accuracy (e.g., which staff review codes, percent of codes reviewed) prior to submitting to payers. Use the review process to identify common mistakes in coding and billing and ensure future education and tools aim to address these errors. Your team may also identify trends in coding errors through a review of revenue cycle reports that require further training.

Flu Vaccine Payment Guidelines
UC San Diego Health
Diagrams patient vaccine payment methods for varying office visit and insurance scenarios.
View Tool
Adult Current Procedural Terminology® (CPT) Coding Case Scenarios
National Adult and Influenza Immunization Summit (NAIIS)
Features several case studies designed to provide healthcare professionals with guidance on appropriate coding and billing for a range of scenarios involving vaccine counseling and/or administration for adult patients.
View Tool
Top Questions on Coding and Billing for Vaccines
National Adult and Influenza Immunization Summit (NAIIS)
Provides answers to common questions regarding the coding and billing of adult vaccinations.
View Tool
Flu Shot Billing
Centers for Medicare and Medicaid Services (CMS)
Features information for healthcare providers including resources for payment, frequency & coverage, billing, coding and additional Medicare and influenza resources.
View Tool
Medicare Part D Vaccines Factsheet
Centers for Medicare and Medicaid Services (CMS)
Details administration coverage for Medicare Part D vaccines. Includes information on a number of patient scenarios to allow providers to distinguish under which plans vaccination administration may be payable.
View Tool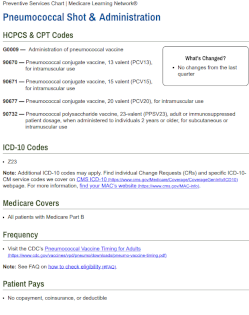
Medicare Preventative Services: Pneumococcal Shot and Administration
Centers for Medicare and Medicaid Services (CMS)
Provides a list of procedure and diagnostic codes for pneumococcal vaccinations as well as information on vaccine eligibility and timing for adult patients.
View Tool
Seasonal Influenza and COVID-19 Vaccines and Pricing
Centers for Medicare and Medicaid Services (CMS)
Provides a listing of Medicare Part B payment allowance limits for seasonal influenza vaccines.
View ToolCampaign Planks
Provider & Staff Education
Clinical Support
IT / Documentation
Patient Education
