Continuous Glucose Monitors in Primary Care

Issue
Rates of type 2 diabetes (T2D) continue to rise in the United States, with many patients failing to achieve glycemic targets. Primary care providers often serve as the sole clinician managing diabetes. Continuous glucose monitors (CGMs) have shown promise in diabetes management, yet their adoption in primary care settings, especially among patients with T2D not using intensive insulin therapy, remains limited.
Project Objective
AMGA Research & Analytics and Piedmont HealthCare (Statesville, NC) sought to evaluate the impact of CGM use on glycemic control in patients with T2D not using insulin and those using basal but not bolus insulin in a primary care setting.
Interventions
Eight primary care clinics at Piedmont HealthCare were trained to utilize CGMs in their practice. Clinic staff viewed a 90-minute webinar on how to implement the Dexcom™ G6 professional and personal CGM systems and received virtual live training. This taught staff how to initiate patients on the CGM systems, obtain CGM reports through Dexcom CLARITY, and troubleshoot issues. Most practice sites relied on medical office assistants (MOAs) to be trained to initiate participants on CGMs. Teams received bi-weekly updates with recruitment goals/achievements and study updates.
Participation in the study offered the following opportunities:
- Building organizational research infrastructure
- Providing professional development for providers and staff
- Improving outcomes for patients
- Aligning with Value-Based Care focus
Results
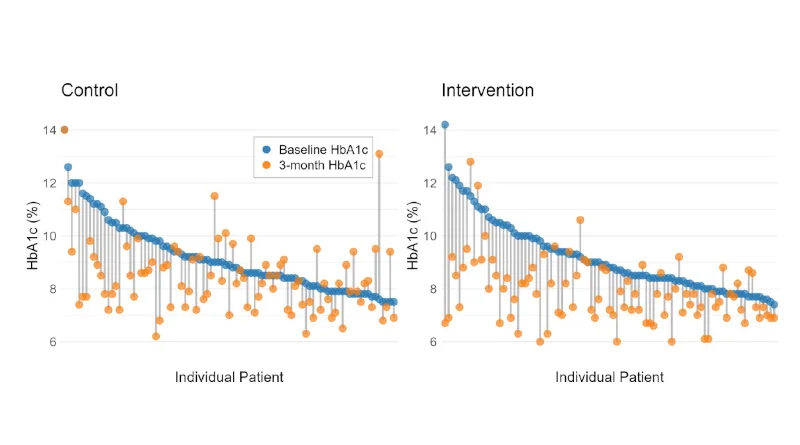
CGM use was associated with a significantly greater reduction in HbA1c (-0.62%) compared with matched controls at 3 months (p<0.01; n=182)). Patients showed significant improvements in time in range (40 to 62%), time > 180 mg/dL (60 to 38%), time > 250 mg/dL (28 to 9%), mean estimated glucose value (212 to 173 mg/dL) and glucose management indicator (8.3 to 7.5%) (all p<0.001).
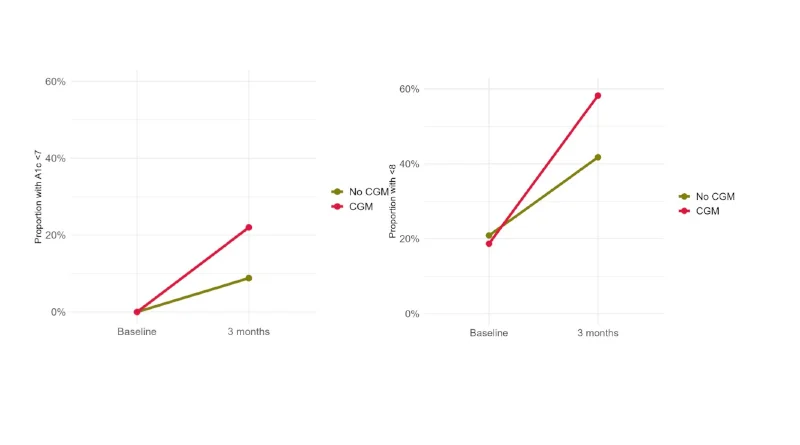
Additionally, in the intervention group, there were 13% more patients with A1c < 7 and 19% more patients with A1c < 8 compared with the controls (p<0.05).
Fig 1: Change (gray line) from baseline A1c (blue) to 3-month A1c (orange) for each patient in the control (left) and intervention (right) groups
Figs 2 & 3: 3-month change in the proportion of patients with A1c control <7% and <8% in the No CGM (green) versus CGM (red) groups
Providers generally found the overall experience favorable and were generally satisfied
- MDs, PAs, MOAs, CCMAs, Office Managers, front office staff completed survey (n=9)
On a 5-point Likert scale (1=Strongly Disagree, 5=Strongly Agree)
| Overall Experience | |
| CGMs made my patient’s management of T2DM easier | 4.3 |
| CGMs improve the quality of T2DM care | 4.3 |
| CGMs take more time and work than it is worth | 2.7 |
| CMGs can benefit all patients with T2DM | 3.8 |
| Satisfaction | |
| Ease of use | 3.7 |
| Usefulness for patients | 4.1 |
| Data format | 3.4 |
| Ability to improve glycemic control | 4.1 |
| Modifying treatment patterns such as visit frequency and medical changes | 3.7 |
Additional project information